i5 Analytics supports Population Health Management (PHM) in the NHS by applying advanced Algorithms and Artificial Intelligence (AI) to a range of services.
Those services include targeted screening programmes for delivering pro-active care, referral recommendations for matching patients to interventions and strategic decision support for planning and transformation of Health economies.
Targeted Screening Programmes - The Atrial Fibrillation Challenge
 Atrial Fibrillation (AF) prevalence estimates for England have been calculated on a whole population using latest known age and sex distributions of AF diagnosed in a Swedish region. The conclusion is that 1.4 million people are living with AF. This means that current estimated prevalence is around 2.5%. More men are expected to be living with AF compared to women, 825,000 versus 580,000. There are however approximately only 985,000 people registered with their GPs as AF sufferers in England. This equates to a diagnosed prevalence rate of 1.7% and suggests that a further 425,000 people are living with undiagnosed AF across England.
Atrial Fibrillation (AF) prevalence estimates for England have been calculated on a whole population using latest known age and sex distributions of AF diagnosed in a Swedish region. The conclusion is that 1.4 million people are living with AF. This means that current estimated prevalence is around 2.5%. More men are expected to be living with AF compared to women, 825,000 versus 580,000. There are however approximately only 985,000 people registered with their GPs as AF sufferers in England. This equates to a diagnosed prevalence rate of 1.7% and suggests that a further 425,000 people are living with undiagnosed AF across England.
i5 has developed algorithms in order to find these unrecognised patients. By applying the i5 Pre-Diagnosis Predictor (PDP) to secondary care data, two groups of individuals have been identified that may not currently receive the appropriate treatment:
The two patient groups that may not currently receive the appropriate treatment:
- Missing Patients: Patients that were diagnosed by a Healthcare professional in secondary care to have an LTC but this has not been communicated to primary care where the patient remains undiagnosed and not treated for their condition (clinically diagnosed but not on the register in primary care)
- Likely Patients: Patients that have a very similar Healthcare history as patients that have the targeted LTC but have not been diagnosed, based on analysis of a large cohort of patients with the condition. In the Haringey borough of North London, AF prevalence was well below the national average and analysis was undertaken to locate missing patients, see below.
Haringey, London - Atrial Fibrillation
In the Haringey borough of North London, AF prevalence lies at 0.76% – which is only 45% of the national average of 1.71%. To reach national average, 5,233 patients would need to be on the AF register, which would require an additional 2,890 patients with the condition to be added to the 2,343 patients already diagnosed.
Over the last three years NHS Haringey’s AF prevalence has grown faster than the national average but the number on the register remains well below that expected based on national averages. Using list size comparison and advanced algorithms, 363 missing and 2,310 likely patients were identified covering three years from 2013/14 to 2016/17. Overall, 2,673 patients were identified and assuming a success ratios of 80%, the AF prevalence could increase to 1.45%, which is 85% of national average.
The i5 AF detection algorithm identified cohorts of undiagnosed AF patients that were provided to the relevant Haringey General Practitioners (GPs) for review. Result: a positive diagnosis rate of 28% (649) observed for patients in the range between 80%-100%. Of the 649 patients identified with AF, approximately 13.9% (90) would have developed a stroke with a health and social care burden of £45,409 in the first year and £24,778 in subsequent years. For 90 patients, apart from poor health, the total cost avoided is £13,021,000 over 5 years with a programme cost of less than £25,000.
The Technology
The technology used to identify patients with a probable diagnosis of Atrial Fibrillation is based on expert systems that can perform a Principal Component Analysis (PCA) to prepare data for training of AI to facilitate Neural Networks to compute the probability of a patient having a condition. Our service Preliminary Diagnosis is able to use your data to identify undiagnosed patients for Atrial Fibrillation, Heart Failure and related conditions.
Saudi Arabia – Atrial Fibrillation
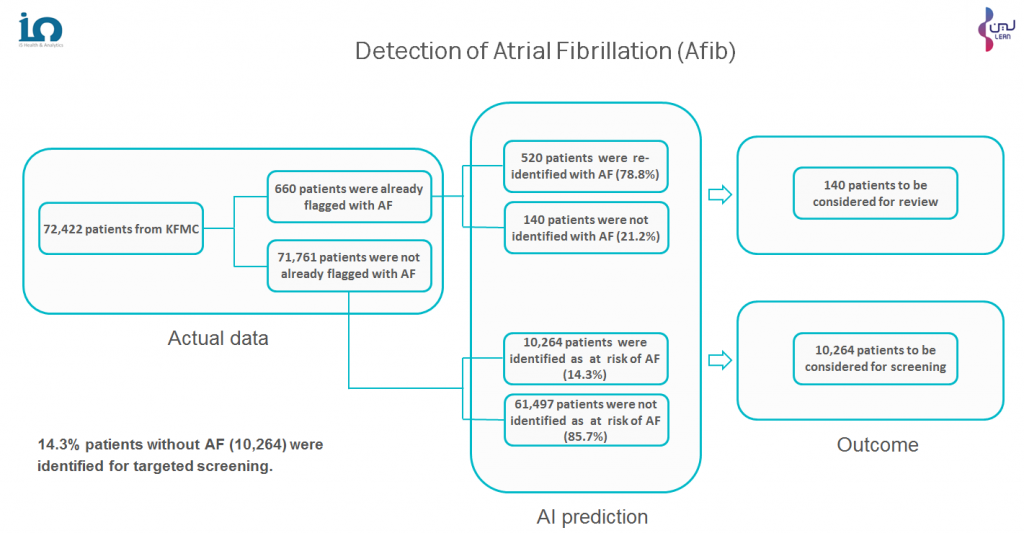
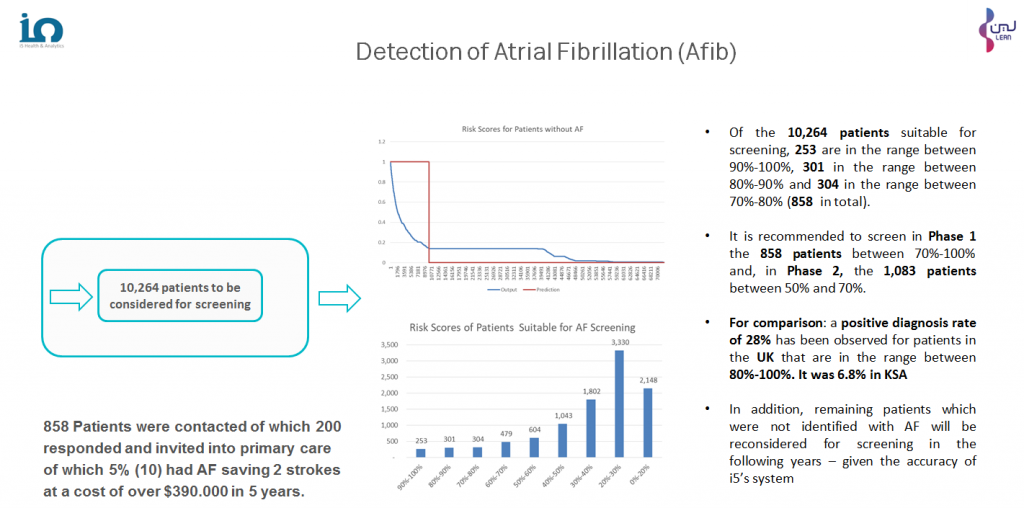
In an exercise carried out with one of the largest hospital groups in the KSA, King Fahad Medical City (KFMC), i5 PDP was applied to the historic medical records of 72,422 patients to establish their risk levels for Atrial Fibrillation (AF). The initial exercise carried out to validate the algorithms being used confirmed a circa 80% accuracy level (compared to 92% in respect of NHS data). The difference was attributed to coding practice. Of the 72,422 patients, 10,264 were identified as suitable for screening. From this cohort, 858 of those with risk levels of 70% and above were invited for screening. Just 200 responded to the invitation and 10 of these were diagnosed with AF and put on care programmes. It is estimated that this action prevented 2 strokes that would otherwise have cost $390,000 over 5 years.
Saudi Arabia – Diabetes
In an ongoing exercise using the data provided by the Ministry of Health of 40 hospitals in the KSA, i5 PDP has been applied to the historic medical records of 491,137 patients to establish their risk levels for Diabetes. The initial exercise validating the algorithms being used confirmed a 78.7 % accuracy level compared to 92% in respect of NHS data and virtually the same for the Atrial Fibrillation exercise with KFMC). The difference between the UK and KSA validations is attributed to coding practice. Of the total number of patients, 74,025 have been identified as suitable for screening. From this cohort, 49,586 of those with risk levels of 80% and above are to be invited for screening.


The Technology
The technology used to identify patients with a probable diagnosis of Atrial Fibrillation is based on expert systems that can perform a Principal Component Analysis (PCA) to prepare data for training of AI to facilitate Neural Networks to compute the probability of a patient having a condition. Our service Preliminary Diagnosis is able to use your data to identify undiagnosed patients for Atrial Fibrillation, Heart Failure and related conditions.
Targeted Screening Programmes – Finding Undiagnosed Patients
 At the request of NHS England, the governing body of the NHS, i5 applied its AI detection system to the 2014/15 Health data for the population within the area covered by Southport & Formby Clinical Commissioning Group (CCG). Nineteen Long Term Conditions (LTCs) were targeted. The results showed that there were, overall, 1,113 patients across thirteen of those conditions categories missing from the GPs registers and 3,182 patients likely to be afflicted with the conditions, or at risk of developing the conditions, if no action was taken.
At the request of NHS England, the governing body of the NHS, i5 applied its AI detection system to the 2014/15 Health data for the population within the area covered by Southport & Formby Clinical Commissioning Group (CCG). Nineteen Long Term Conditions (LTCs) were targeted. The results showed that there were, overall, 1,113 patients across thirteen of those conditions categories missing from the GPs registers and 3,182 patients likely to be afflicted with the conditions, or at risk of developing the conditions, if no action was taken.
The Southport & Formby GPs took action and the 2015/16 Population Management QOF Register, which expanded by over 3,000 against the previous year, showed that a number of the 2014/15 “missing” and “likely” patients identified by i5 were diagnosed or registered and therefore able to receive the treatment they needed.
The Technology
The technology used to identify patients in the example above was based on expert systems that can perform a Principal Component Analysis (PCA) to prepare data for training of AI to facilitate Neural Networks to compute the probability of a patient having a condition. Our service Preliminary Diagnosis is able to use your data to identify undiagnosed patients for over 20 Long Term Conditions and calculate the risks of developing complications e.g. diabetic ulcers.
Referral Recommendations - Social Prescribing for London
 Social Prescribing (SP) is a method whereby patients are identified for non-pharmaceutical prescribing in primary care. Such prescribing includes initiatives like Arts on Prescription, Ecotherapy for Substance Abuse patients and Exercise on Prescription.
Social Prescribing (SP) is a method whereby patients are identified for non-pharmaceutical prescribing in primary care. Such prescribing includes initiatives like Arts on Prescription, Ecotherapy for Substance Abuse patients and Exercise on Prescription.
At the request of NHS England (the governing body of the NHS), i5 has carried out an exercise to identify and economically evaluate NHS services in London that could support patients who would benefit from SP locally. Based on this, potential savings from reduced secondary care use were quantified. These savings were identified for each of the 32 London Clinical Commissioning Groups (CCGs) and 5 London Sustainability and Transformation Partnership (STP) footprints as well as for the whole of London itself.
In consequence, the CEO of NHS England, Simon Stevens, requested that, in order to implement a new operating model, i5 develop “Cohort Identification” information to support practices at the beginning of the pathway and to calculate, for each practice, financial investment and returns should the identified patients use the SP interventions.
i5 has delivered bespoke reports to all 5 London STPs and the 32 CCGs down to GP surgery level as well as individual Dashboards for use in the one year and five year planning exercises. Over 60% of the London's 32 CCGs have used the system for their one year and five year plans; over 50% of the CCGs in London are using it to support funding applications under the Department of Health and Public Health England VCSE grants system. i5 is now working with the NEL Commissioning Support Unit and NHS Digital on the identification of specific individuals within cohorts for referral recommendations.
The Technology
The technology used to match patients to the most appropriate Social Prescribing (SP) services is based on published evidence that is used to perform a Principal Component Analysis (PCA) to prepare data for training of AI to facilitate Neural Networks to recommend SP services for patients. Our services Planning and Service Redesign and Referral Recommendations are able to use your data to match patients to over 400 Out-Of-Hospital services to enable you to identify missing or under-capacity services for Service Redesign.
A sample dashboard summarising the Social Prescribing opportunities in London can be accessed here:
Go to Social Prescribing Economic Impact Dashboard
Strategic Decision Support - Digital Healthcare for London
 The London Digital Programme, which is part of The Healthy London Partnership (HLP) of NHS England, commissioned i5 to produce an economic modelling tool to support implementation of digitally enabled new models of care.
The London Digital Programme, which is part of The Healthy London Partnership (HLP) of NHS England, commissioned i5 to produce an economic modelling tool to support implementation of digitally enabled new models of care.
The result is a package of 48 evidence based technology solutions which are explored in detail in the main report in terms of their potential to release efficiencies. In addition, the data used is plugged into a dashboard tool configured to the 5 populations of the STP footprints across London. The explicit intention is for STP leads to use the tool to work through the potential benefits of transforming the traditional face to face and paper heavy workflows across primary and secondary care into digital workflows and to assist with decision making and prioritization. Examples include implementing virtual triage, e-consultations, artificial intelligence, decision – support, electronic alerts and notifications, use of big data and self -management tools.
The main conclusion is that the 48 technology enabled initiatives could release financial values annually totalling over £700m in the fifth year for the capital’s NHS through the associated impacts on workflows, workforce and estates. The initiatives fall in into two principal categories:
- Those that replace a face to face events with a digital alternative, known as ‘channel shift’
- Those that replace a human process with a digital one or create a new digital process where there was previously no human equivalent
Each NHS organisation in London (CCGs, STPs and Acute Trusts) now has access to the reports relevant to their areas and activities to plan their digital strategy for over 9 million people.
The Technology
The technology used to match patients to the most appropriate Digital services is based on published evidence that is used to perform a Principal Component Analysis (PCA) to prepare data for training of AI to facilitate Neural Networks to recommend Digital services for patients. Our services Planning and Service Redesign and Referral Recommendations are able to use your data to match patients to over 100 Digital services to enable you to identify missing or under-capacity services for Service Redesign.
A sample dashboard summarising the digital opportunities in London can be accessed here:
Go to Digital Economic Impact Dashboard
Strategic Decision Support – Regional Transformation Support
 Arden & GEM Commissioning Support Unit (AGEM CSU) provides a wide range of commissioning support services to multiple customers across the Midlands, North West, East Anglia and South East England - including NHS England, Clinical Commissioning Groups (CCGs), acute hospital trusts and local governments.
Arden & GEM Commissioning Support Unit (AGEM CSU) provides a wide range of commissioning support services to multiple customers across the Midlands, North West, East Anglia and South East England - including NHS England, Clinical Commissioning Groups (CCGs), acute hospital trusts and local governments.
Besides being a preferred supplier to CSUs, i5 is an Information and Transformation partner of AGEM CSU. The CSU engages i5 to apply, amongst other services, the COP module for CCG customers in Birmingham and the East Midlands. To that end i5 COP algorithms match patient needs to services including but are not limited to Primary Care, A&E, Admissions, MH, Care Homes, Community Care, End of Life, Home Care, Self-Care and Social Prescribing. By using COP, commissioners are supported during the Strategic and Operational Planning stages:
- Strategic Planning: commissioners benefit from a very detailed report that is based on patients’ clinical needs matched to clinical services implemented elsewhere in the NHS.
- Operational Planning: precise calculations are performed that evaluate the opportunity cost based on patient clinical needs. Those opportunity costs support commissioners with developing the business case and the ROI calculations for each service in the short and long term.
In the last year alone, i5 has supplied AI based COP services, through AGEM CSU, to more than a dozen CCGs – some along with i5 workshops to apply the findings to their local Health economy. The COP services provided have included full analysis of their local Healthcare System, patient lists for Population Health Management, Winter reports and Specialised Commissioning reports.
The Technology
The technology used to support Arden & GEM Commissioning Support Unit to match patients to the most appropriate of the hundreds of out-of-hospital services available is based on published evidence that is used to perform a Principal Component Analysis (PCA) to prepare data for training of AI to facilitate Neural Networks to recommend out-of-hospital services for patients. Our services Planning and Service Redesign and Referral Recommendations are able to use your data to match patients to over 400 out-of-hospital services to enable you to identify missing or under-capacity services for regional Service Redesign.
Strategic Decision Support – Local Transformation Support
 Halton Clinical Commissioning Group (CCG) and Halton Borough Council (BC) have been acutely aware that they are working within scarce resources and that, up to and including the year 2019, they and their partners face significant financial challenges. These financial challenges have driven them to do things differently and transform all aspects of Health, social care and wellbeing in Halton over a five year period, beginning with an ambitious 5-year strategy and robust 2 year operational delivery plan. It was into this difficult context that i5 was asked to work with Senior Management on identifying and evaluating QIPP and other ambitions for the purposes of the strategy and plan.
Halton Clinical Commissioning Group (CCG) and Halton Borough Council (BC) have been acutely aware that they are working within scarce resources and that, up to and including the year 2019, they and their partners face significant financial challenges. These financial challenges have driven them to do things differently and transform all aspects of Health, social care and wellbeing in Halton over a five year period, beginning with an ambitious 5-year strategy and robust 2 year operational delivery plan. It was into this difficult context that i5 was asked to work with Senior Management on identifying and evaluating QIPP and other ambitions for the purposes of the strategy and plan.
Halton CCG was planning to find £4.8 million of QIPP savings. Of this £4.8m, £2.6m were taken out of budgets leaving a balance of £2.2m savings to be found in year. In the main they were to be from savings in non-elective and accident and emergency pathways due to the opening of the urgent care centres within Widnes and Runcorn (£1.1m NEL, £0.480m A&E and £0.178m Direct Access).
The Approach
Highly experienced i5 team members, with the relevant experience and skill sets, spent time reviewing and discussing the existing QIPP plans and other ambitions on site with executives and then applied the COP module to the appropriate data in order to establish priority initiatives and their likely outcomes.
In its subsequent ‘5 Year Strategy and 2 Year Operational Plan 2014-2019’, Halton CCG stated:
“NHS Halton CCG commissioned two organisations, i5 and Capita, to provide a detailed analysis of where opportunities existed for the Health economy in Halton to change to provide services which provided better outcomes and better value for money and ensured that acute services were only used by people in acute need. The analysis highlighted that both A&E attendances and Hospital admissions for certain conditions were the significant areas where opportunities for change existed”
In a later published document, the CEO for Halton CCG and Halton BC went on to state:
“Unlike any other piece of consultancy, i5 and COP shone an economic light on what schemes are working well and what areas we could prioritise our energy on”.
According to the Senior Management team, since that initial engagement, the regular use of i5 COP and its drill down reports have become fundamental to decision making within Halton CCG and Halton BC.
The Technology
The technology used to support Halton ICB and Halton Council to match patients to the most appropriate of the hundreds of out-of-hospital services available is based on published evidence that is used to perform a Principal Component Analysis (PCA) to prepare data for training of AI to facilitate Neural Networks to recommend out-of-hospital services for patients. Our services Planning and Service Redesign and Referral Recommendations are able to use your data to match patients to over 400 out-of-hospital services to enable you to identify missing or under-capacity services for local Service Redesign.